Understanding High Blood Pressure -- the Basics
High blood pressure, also known as hypertension, is the most common cardiovascular disease.
If you have high blood pressure, you'll probably find out about it during a routine checkup. Or, you may have noticed a problem while taking your own blood pressure. But be sure to see your doctor for a definite diagnosis, and take the opportunity to learn what you can do to bring your blood pressure under control.
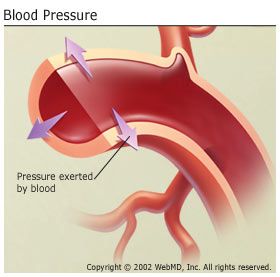
Blood pressure refers to the force of blood pushing against artery walls as it courses through the body. Like air in a tire or water in a hose, blood fills arteries to a certain capacity. Just as too much air pressure can damage a tire or too much water pushing through a garden hose can damage the hose, high blood pressure can threaten healthy arteries and lead to life-threatening conditions such as heart disease and stroke.
Hypertension is the leading cause of stroke and a major cause of heart attack. In the U.S. alone, over 74 million people have high blood pressure.
How Is Blood Pressure Measured?
A blood pressure reading appears as two numbers. The first and higher of the two is a measure of systolic pressure, or the pressure in the arteries when the heart beats and fills them with blood. The second number measures diastolic pressure, or the pressure in the arteries when the heart rests between beats.
Normal blood pressure rises steadily from about 90/60 at birth to about 120/80 in a healthy adult. If someone were to take your blood pressure immediately after you'd delivered a speech or jogged five miles, the reading would undoubtedly seem high. This is not necessarily cause for alarm: It's natural for blood pressure to rise and fall with changes in activity or emotional state.
It's also normal for blood pressure to vary from person to person, even from one area of your body to another. But when blood pressure remains consistently high, talk with your doctor about treatment. Consistently high blood pressure forces the heart to work far beyond its capacity. Along with injuring blood vessels, hypertension can damage the brain, eyes, and kidneys.
People with blood pressure readings of 140/90 or higher, taken on at least two occasions, are said to have high blood pressure. If the pressure remains high, your doctor will probably begin treatment. People with blood pressure readings of 200/120 or higher need treatment immediately. People with diabetes are treated if their blood pressure rises above 130/80, since they already have a high risk of heart disease.
Researchers identified people with blood pressures slightly higher than 120/80 as a category at high risk for developing hypertension. This condition is called prehypertension and affects an estimated 50 million American men and women. Prehypertension is now known to increase the likelihood of damage to arteries and the heart, brain, and kidneys, so many doctors are now recommending early treatment, though there is no evidence that this helps in the long run.
Even so, many people with high blood pressure don't realize they have the condition. Indeed, hypertension is often called "the silent killer" because it rarely causes symptoms, even as it inflicts serious damage to the body. Left untreated, high blood pressure can lead to vision problems, as well as to heart attack, stroke, and other potentially fatal conditions, including kidney failure.
Hypertension may also lead to heart failure, a common but disabling condition that can cause breathing problems. Patients who have very high blood pressure are said to have malignant hypertension, with a diastolic pressure usually exceeding 130 or a systolic pressure above 200. Malignant hypertension is a dangerous condition that may develop rapidly and cause organ damage quickly -- it requires immediate medical attention.
Fortunately, high blood pressure can be controlled effectively. The first step is to have your blood pressure checked regularly.
Who Gets Hypertension?
High blood pressure is more likely in people who:
- Have a family history of high blood pressure, heart disease, or diabetes
- Are black
- Are greater than age 55
- Are overweight
- Are not physically active
- Drink excessively
- Smoke
- Eat foods high in saturated fats or salt
- Use certain medications such as NSAIDs, decongestants, and illicit drugs such as cocaine
What Causes High Blood Pressure?
Essential Hypertension
In as many as 95% of reported high blood pressure cases in the U.S., the underlying cause cannot be determined. This type of high blood pressure is called essential hypertension.
Though essential hypertension remains somewhat mysterious, it has been linked to certain risk factors. High blood pressure tends to run in families and is more likely to affect men than women. Age and race also play a role. In the U.S., blacks are twice as likely as whites to have high blood pressure, although the gap begins to narrow around age 44. After age 65, black women have the highest incidence of high blood pressure.
Essential hypertension is also greatly influenced by diet and lifestyle. The link between salt and high blood pressure is especially compelling. People living on the northern islands of Japan eat more salt per capita than anyone else in the world and have the highest incidence of essential hypertension. By contrast, people who add no salt to their food show virtually no traces of essential hypertension.
Many people with high blood pressure are "salt sensitive," meaning that anything more than the minimal bodily need for salt is too much for them and increases their blood pressure. Other factors that have been associated with essential hypertension include obesity; diabetes; stress; insufficient intake of potassium, calcium, and magnesium; lack of physical activity; and chronic alcohol consumption.
Secondary Hypertension
When a direct cause for high blood pressure can be identified, the condition is described as secondary hypertension. Among the known causes of secondary hypertension, kidney disease ranks highest. Hypertension can also be triggered by tumors or other abnormalities that cause the adrenal glands (small glands that sit atop the kidneys) to secrete excess amounts of the hormones that elevate blood pressure. Birth control pills -- specifically those containing estrogen -- and pregnancy can boost blood pressure, as can medications that constrict blood vessels.






















